Kidney Palliative Care
Improving quality of life
Making a case for Palliative Care
Help us grow the palliative care program! Find out how your donation can help.
News about our Palliative Care program
- Kidney Dialysis Palliative Care Program Bridging a Gap to Hospice
October 2021, Hospice News - ‘My time to live’: Novel program gives Seattle-area kidney patients palliative care and dialysis until the end
September 2021, Seattle Times
Learn more about palliative care.

The Shaw family’s experience
The palliative care team met Louis Shaw and his family in 2018 soon after Louis was diagnosed with cancer.
Louis had a large family, 16 kids spread across the county, and loved to tell staff and other patients stories about those kids. The team reached out as many of the children as they could to tell them about the seriousness of Louis’ condition and to organize an in-person meeting at his residence.
At the family meeting, youngest son and Burien resident Ian was elected to be Louis’ Durable Power of Attorney. The team began guiding Ian in his new role, while separately meeting weekly with Louis about his goals and needs.
Louis, who had been told he was too weak to survive chemotherapy, chose to get healthier and stronger. In 2019 was deemed strong enough to start chemotherapy.
As he got stronger, he met less often with the Palliative Care team, and began participating more in the activities he enjoyed and spending time with his family. Having always loved to sing, he joined the choir at his nursing home. Bingo became another pastime. One of Louis’ favorite days was when a group of his kids came and took him out fishing, a favorite pastime that he hadn’t been able to do in years.
COVID-19 restrictions cut Louis off from a lot of personal contact. Though his family spoke with him regularly by phone, in person visits were not allowed. When Ian saw Louis again in person, he did not think that Louis looked healthy, and he feared the worst: the chemotherapy was not working.
“Nobody wants to have that conversation. They [the team] really helped me,” said Ian, about the counsel he received at that time.
The team began meeting with Louis regularly, giving him reprieve from the distancing and isolation from COVID-19 restrictions. In spite of masks and personal protective equipment, “you could feel the warmth in those visits” said Jennifer Christophel Lichti.
During his last year, Louis survived COVID-19 but ultimately succumbed to the cancer in fall 2020. The palliative care team was again able to support Ian and the family during that time.
“After Pops passed away, Jennifer checked on me every month or so to talk and see if I was okay. Of course, I wasn’t, but it really helped. Then one day she called, and I told her I thought I was better. She said I sounded better. And I was feeling better,” said Ian. “She still checks in once in a while.”
Kidney Palliative Care team
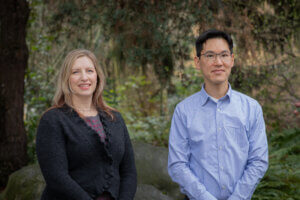
 Daniel Lam, MD, Medical Director
Daniel Lam, MD, Medical Director
Dr. Lam is a Clinical Associate Professor of Medicine at the University of Washington and serves as the Palliative Care Medical Advisor for Northwest Kidney Centers. He believes that understanding each person’s story is vital to individualizing care. Dr. Lam’s interest in palliative care was motivated by personal experiences with the health care system, and he is especially interested in bringing palliative care to people living with kidney disease to improve their lives. His work as a 2015 Sojourns Scholar to improve palliative care access for people living with kidney disease evolved into the Kidney Palliative Care Program. Dr. Lam is board certified in Internal Medicine, Palliative Medicine, and Nephrology.
 Megan Nolan, RN, BSN, Program Supervisor
Megan Nolan, RN, BSN, Program Supervisor
Through 19 years of experience as a critical care nurse and palliative care nurse, she has found a passion for enhancing quality of life for people with serious illness. She also believes in the importance of fostering healthy work environments for health care professionals. Her professional goal is to collaborate with patients, families and other health care professionals to provide person-centered care and communication. She engages in on-going professional development and quality improvement to seek out best practices and optimal care delivery pathways. She holds a Bachelor of Science in Nursing from the University of Rochester and a Graduate Certificate in Palliative Care from the University of Washington.